Keratoconus is a progressive condition that affects the clarity and shape of the cornea, gradually altering the way light enters the eye. Over time, it can significantly impact a person’s visual quality and daily activities if left untreated. While the condition may sound intimidating, advancements in diagnostic technology and modern therapeutic approaches now allow for effective management and long-term stabilization. This article aims to explain what keratoconus is, why it develops, how it is diagnosed, and the full range of treatment options available today.
What is Keratoconus?
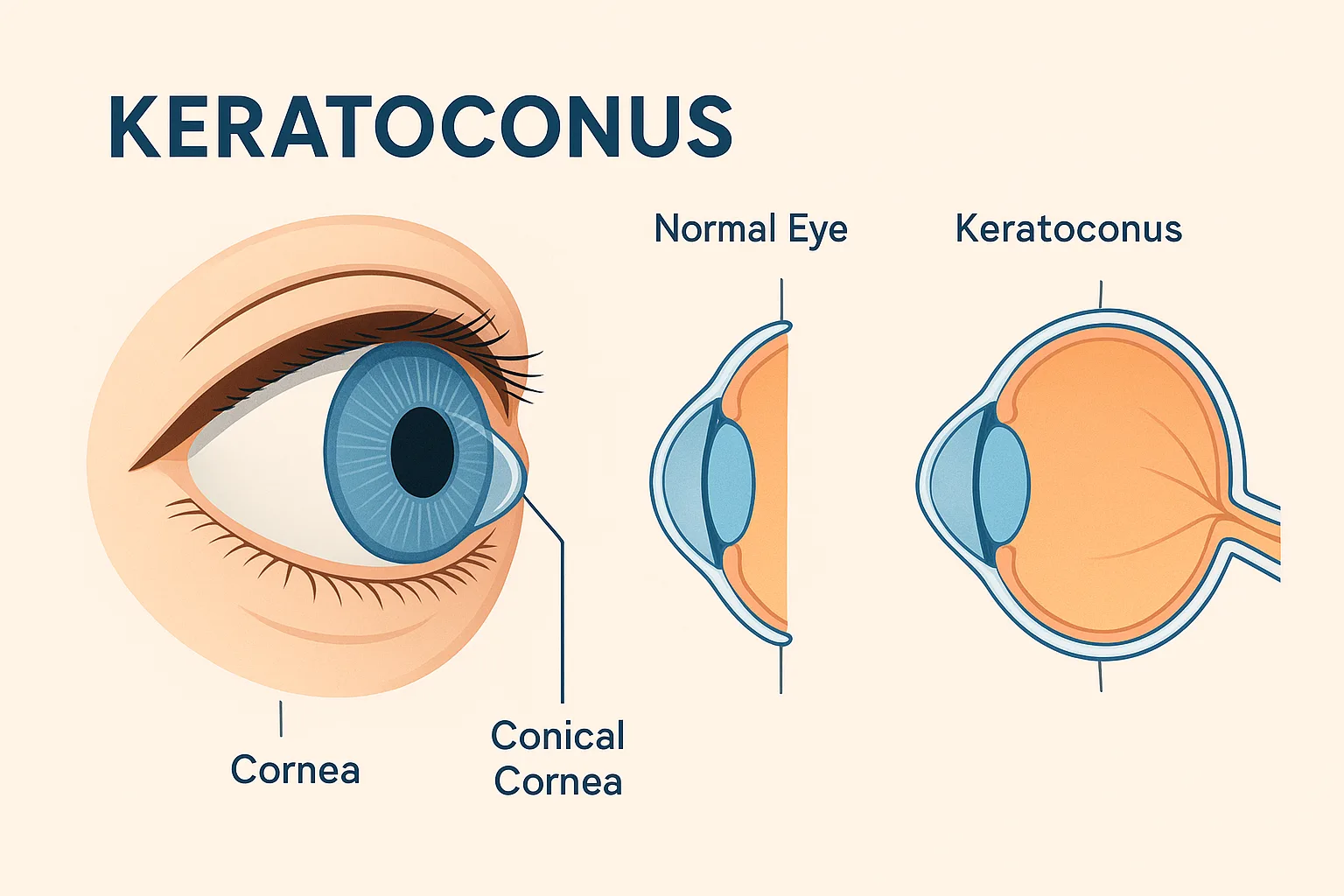
The cornea is the transparent front window of the eye responsible for focusing incoming light. In a healthy eye, it maintains a smooth, dome-like shape. In keratoconus, however, the cornea gradually becomes thinner and begins to bulge outward into a cone-shaped structure. This irregular shape disrupts light refraction, often resulting in distorted or blurred vision. The condition usually begins in adolescence or early adulthood and may progress for many years before stabilizing.
Although the exact cause remains unclear, research suggests a combination of genetic, biochemical, and environmental factors. The condition can affect one or both eyes, though the degree of progression often differs between sides.
Underlying Causes and Risk Factors
While no single cause has been identified, several risk factors are widely recognized:
Genetic predisposition
Studies show that keratoconus may run in families. Individuals with a close relative diagnosed with this corneal disorder are at higher risk of developing it themselves.
Chronic eye rubbing
Persistent rubbing of the eyes—commonly associated with allergies, eczema, or habitual behavior—has been strongly linked to corneal weakening. The mechanical stress can contribute to progressive thinning.
Atopic conditions
People with asthma, allergic conjunctivitis, eczema, or other atopic diseases may be more prone to developing corneal changes due to chronic inflammation.
Connective tissue disorders
Certain systemic conditions involving collagen abnormalities are associated with a higher incidence of keratoconus.
Oxidative stress
Biochemical imbalances in the cornea may play a role in weakening its structural integrity over time.
Identifying and addressing the modifiable factors—especially eye rubbing—can significantly slow progression and protect vision.
Common Symptoms Patients Experience
Keratoconus typically begins with subtle changes that may be mistaken for routine refractive shifts. Over time, symptoms become more noticeable:
- Blurred or distorted vision
- Increased sensitivity to light or glare
- Frequent changes in eyeglass prescription
- Difficulty seeing clearly at night
- Double or ghosting images in one eye
- Eye strain and headaches
- Reduced contrast sensitivity
- Halos around lights
As the cornea becomes more irregular, standard glasses may no longer provide satisfactory vision, and more advanced optical solutions become necessary.
How Keratoconus is Diagnosed
Early detection is essential for preventing long-term visual impairment. Today’s diagnostic tools are highly sensitive, allowing ophthalmologists to identify even the earliest signs.
Corneal topography
This non-invasive imaging technique maps the curvature of the cornea. It is the gold standard for detecting irregularities associated with keratoconus.
Tomography
Advanced imaging such as Scheimpflug or OCT-based tomography provides 3D analysis of the cornea, including thickness measurements and posterior curvature changes, often revealing early progression.
Pachymetry
This test measures corneal thickness. Thinning in characteristic patterns can indicate early stages of the condition.
Refraction and visual acuity tests
Frequent changes in astigmatism or myopia may signal corneal instability.
Slit-lamp examination
The ophthalmologist may observe subtle corneal findings such as thinning, scarring, or Fleischer rings.
Regular monitoring with these technologies is crucial for timely intervention.
Modern Treatment Options
Although keratoconus is a chronic condition, modern ophthalmology offers a wide range of treatments that can stabilize the cornea, enhance visual clarity, and prevent severe vision loss.
1. Cross-Linking (CXL)
Corneal cross-linking is currently the only treatment proven to halt or slow progression. This minimally invasive procedure strengthens corneal collagen fibers through the application of riboflavin and controlled ultraviolet light. It increases the biomechanical stability of the cornea, reducing the risk of further bulging. Most patients resume daily activities within a short recovery period.
2. Specialized Contact Lenses
When glasses no longer provide clear vision, advanced contact lens technologies can help:
- Rigid gas-permeable lenses: Provide a smooth refractive surface.
- Hybrid lenses: Combine the clarity of rigid lenses with the comfort of soft lenses.
- Scleral lenses: Vault over the irregular cornea and rest on the sclera, offering excellent vision and comfort for advanced cases.
- Custom soft lenses: Designed specifically for early-stage irregularities.
These options are selected based on the corneal shape, severity, and patient comfort preferences.
3. Intracorneal Ring Segments (ICRS)
Small, curved implants are inserted into the corneal stroma to reshape the cornea and improve visual quality. They can reduce irregular astigmatism and improve tolerance to glasses or contact lenses. They are particularly useful for patients who are no longer achieving satisfactory vision correction with lenses alone.
4. Photorefractive Procedures in Selected Cases
In carefully selected patients with stable corneal structure—often after cross-linking—surface laser procedures may be used to improve vision. These are performed cautiously and are not suitable for every case.
5. Corneal Transplantation
In advanced stages with corneal scarring or significant thinning, transplant procedures such as deep anterior lamellar keratoplasty (DALK) or full-thickness transplantation may be required. Fortunately, the need for transplant surgery has decreased significantly thanks to widespread adoption of early cross-linking.
Long-Term Outlook and Importance of Follow-Up
Most individuals with keratoconus maintain functional vision throughout their life when the condition is detected early and managed correctly. Regular follow-ups are essential, especially for individuals under 30, as progression tends to be more rapid in younger patients.
Avoiding eye rubbing, treating allergic eye disease, and following personalized management plans all contribute to long-term stability. With modern treatment options, the vast majority of patients can achieve excellent visual function without needing major surgery.
Living with Keratoconus
While receiving the diagnosis can be overwhelming, knowledge and early intervention are powerful tools. Patients can continue their daily routines—work, reading, driving, and digital activities—with appropriate management. From cross-linking to advanced contact lenses, today’s treatments offer a full spectrum of solutions tailored to individual needs.