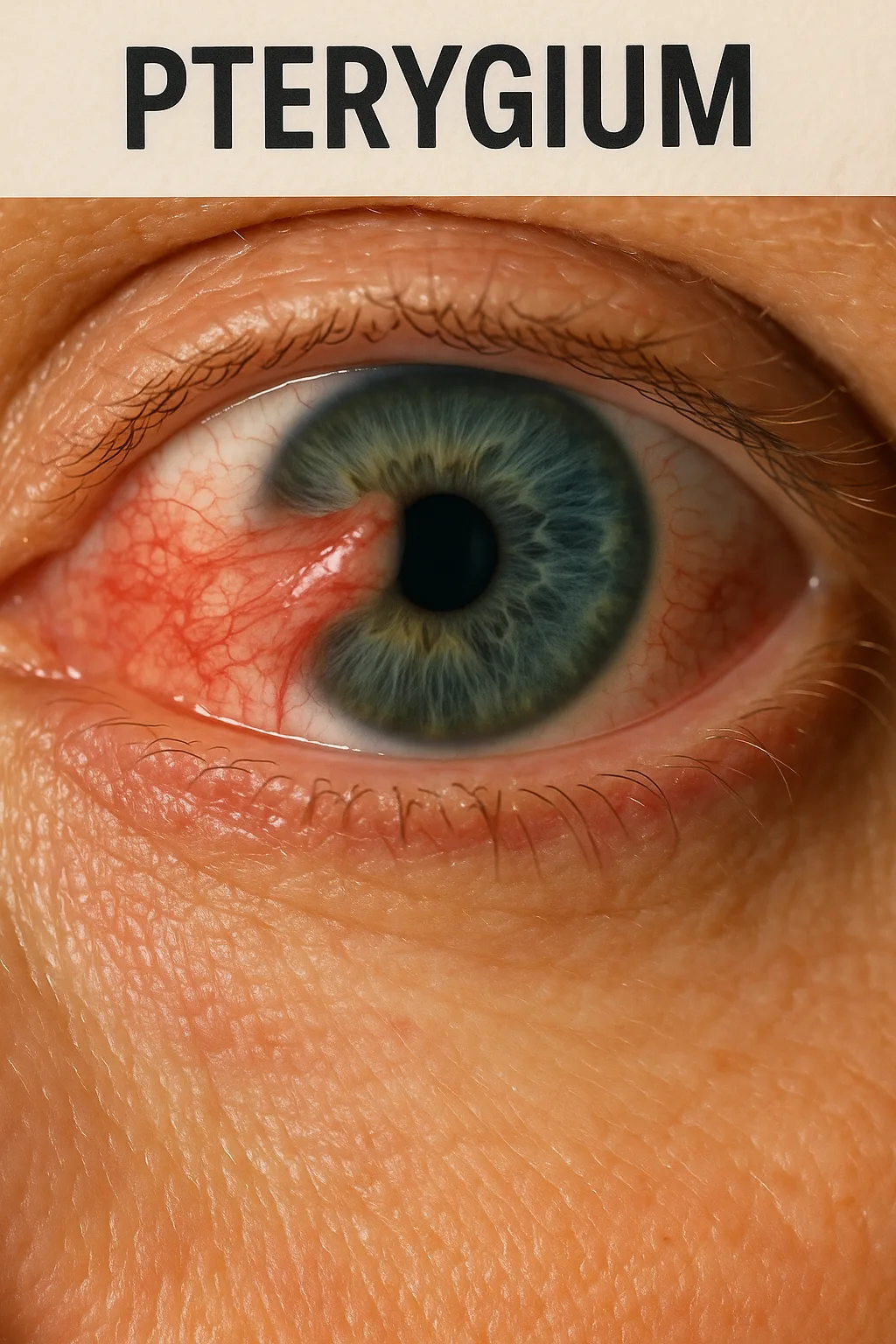
Pterygium is a common, non-cancerous eye condition characterized by the growth of a fleshy, triangular-shaped tissue on the conjunctiva that can extend onto the cornea. This lesion typically forms on the nasal side of the eye and may progress toward the center of the cornea over time, potentially interfering with vision. The condition gets its name from the Greek word pterygion, meaning “little wing,” due to its wing-like shape.
Though pterygium is generally benign, it can cause irritation, redness, tearing, cosmetic disfigurement, and even visual impairment if the growth reaches the central cornea or induces significant astigmatism.
Causes and Risk Factors
The exact cause of pterygium remains unknown, but several environmental and genetic factors have been strongly associated with its development. The most significant among these are:
- UV Light Exposure: Prolonged exposure to ultraviolet radiation, particularly in individuals living in tropical or equatorial climates, is the leading risk factor.
- Chronic Irritation: Wind, dust, sand, and smoke can irritate the ocular surface and increase the likelihood of pterygium development.
- Dry Eyes: Patients with insufficient tear production or poor tear film quality are more prone to pterygium.
- Genetic Factors: Family history of pterygium may play a role, especially in populations with darker iris pigmentation.
- Occupational Exposure: Outdoor workers such as farmers, fishermen, and construction workers are at increased risk due to continuous exposure to sun, dust, and wind.
Protective measures, such as wearing sunglasses with UV protection and using artificial tears, can reduce the incidence of the condition.
Symptoms and Signs
Pterygium may be asymptomatic in its early stages. As the lesion progresses, it often leads to:
- Redness and Irritation: Chronic inflammation due to the exposure of the ocular surface.
- A Visible Growth: The hallmark of pterygium is a fleshy, elevated lesion that may increase in size over time.
- Dryness or Grittiness: The affected eye may feel like there’s something in it.
- Blurred Vision: If the growth invades the central cornea or induces astigmatism.
- Foreign Body Sensation: Especially during blinking or windy conditions.
- Cosmetic Discomfort: Especially in visible or advanced cases, the appearance may be bothersome.
While the lesion itself is benign, symptoms can significantly impact quality of life, particularly in recurrent cases.
Diagnosis
Diagnosis of pterygium is typically clinical and involves:
- Slit-Lamp Examination: To assess the size, shape, and extent of the lesion.
- Corneal Topography: To measure changes in the shape of the cornea and determine whether the pterygium is affecting vision.
- Photography: Baseline images may be taken to monitor the lesion over time.
In rare cases, a biopsy may be recommended to rule out malignancies, especially in atypical or rapidly growing lesions.
Treatment Options
Treatment depends on the size, symptoms, and progression of the lesion. The goals are to relieve symptoms, improve cosmesis, and prevent recurrence or vision loss.
Conservative (Non-Surgical) Treatment
Mild or early-stage cases can often be managed without surgery:
- Lubricating Eye Drops: Help reduce dryness and irritation.
- Anti-inflammatory Drops: Corticosteroid or NSAID eye drops can be used to control inflammation.
- UV Protection: Wearing wraparound sunglasses is highly recommended.
- Environmental Modifications: Avoiding exposure to dust, smoke, and wind can prevent further irritation.
While these approaches may alleviate symptoms, they do not eliminate the growth.
Surgical Treatment
Surgery is the definitive treatment for pterygium and is considered in the following scenarios:
- Cosmetic disfigurement
- Visual impairment due to astigmatism or encroachment on the visual axis
- Recurrent inflammation or discomfort
Surgical Techniques Include:
- Bare Sclera Excision: Simple removal of the pterygium; high recurrence rate.
- Conjunctival Autograft: The preferred method where healthy tissue is transplanted to the excised area to reduce recurrence.
- Amniotic Membrane Graft: Used in cases with limited conjunctiva or recurrence.
- Use of Adjunctive Therapies: Mitomycin C or anti-VEGF injections may be used to lower the recurrence rate.
Post-operative care is critical and includes antibiotic-steroid drops, UV protection, and regular follow-ups.
Prognosis and Recurrence
Most patients recover well after pterygium surgery, with relief from both cosmetic and functional issues. However, recurrence is a major concern, particularly in young patients and those who do not adhere to UV protection post-surgery. Recurrence rates can vary widely:
- Bare sclera technique: Up to 80%
- Conjunctival autograft: Around 5–15%
- Adjunctive therapies reduce recurrence further
Long-term preventive measures are key to maintaining surgical success.
Lifestyle Impact
Though often overlooked, pterygium can affect a patient’s quality of life:
- Work Efficiency: Especially for outdoor workers, eye discomfort may impair productivity.
- Appearance: Visible growth can lead to self-consciousness.
- Vision: Astigmatism and dry eye can reduce reading, driving, or screen usage comfort.
- Mental Health: Recurrent irritation or cosmetic anxiety may contribute to stress.
Counseling and education about sun protection and eye hygiene play an important role in patient well-being.
Differential Diagnosis
Several other ocular conditions may mimic pterygium:
- Pinguecula: A yellowish bump on the conjunctiva that does not invade the cornea.
- Conjunctival Nevus: Typically pigmented, unlike the fleshy appearance of pterygium.
- Conjunctival Squamous Cell Carcinoma: Malignant and may resemble a pterygium—requires biopsy.
- Limbal Dermoid: Congenital growth, usually involving the limbus.
Correct diagnosis ensures appropriate treatment and eliminates unnecessary concern.
Emerging Treatments and Research
Advances in surgical techniques and pharmaceuticals continue to improve outcomes. Ongoing studies are investigating:
- Fibrin glue instead of sutures for faster healing and less discomfort.
- Anti-fibrotic agents to inhibit recurrence at the cellular level.
- Customized UV-blocking contact lenses as a preventive strategy.
- Gene expression profiling to understand susceptibility and growth potential.
As ophthalmic research progresses, patient-tailored treatment becomes increasingly feasible.
FAQs
Can pterygium cause blindness?
Not typically. However, in advanced cases it may obscure the pupil or distort the cornea enough to cause significant visual impairment.
Is surgery painful?
Pterygium surgery is generally performed under local anesthesia. Most patients experience only mild post-operative discomfort.
Does pterygium return after surgery?
It can, particularly if UV exposure is not managed. However, modern surgical techniques have greatly reduced recurrence rates.
Can I use herbal or natural remedies?
There is no proven natural treatment that can remove a pterygium. Medical treatment is advised.
Conclusion
Pterygium is a common eye condition associated with sun exposure, environmental irritation, and genetic predisposition. While often harmless, it can lead to significant discomfort, cosmetic concerns, and visual impairment. Early detection and protective measures, such as UV shielding and artificial tears, can prevent or slow its progression. When necessary, surgical excision with autograft remains the gold standard for treatment. By understanding and addressing the condition proactively, patients can maintain both eye health and quality of life.